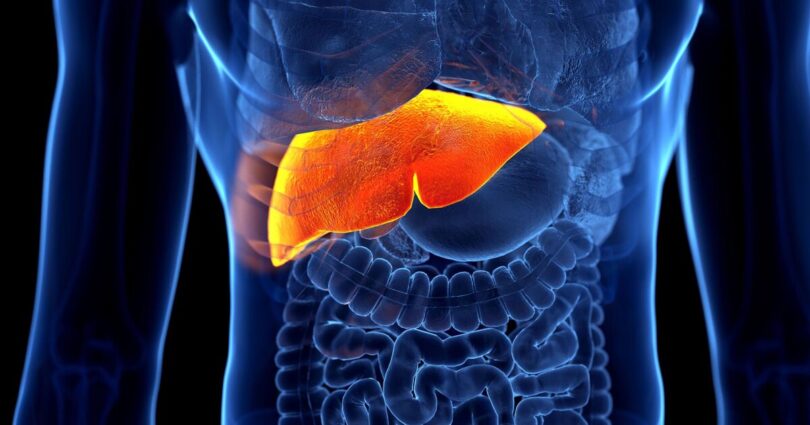
Our liver performs hundreds of jobs essential to health and wellbeing. It processes and helps convert digested food into energy, stores vital nutrients for when we need them, cleans the blood of toxins, regulates blood clotting and much more.
So, it’s crucial you take care of it, especially since liver disease can affect anyone and is becoming more common. One in three of us is at risk of liver disease and the numbers of people being diagnosed have been increasing at an alarming rate,” says Pamela Healy, chief executive of the British Liver Trust.
While some causes of liver disease, like genetics and autoimmune conditions, are beyond our control, there are other risk factors where we can take steps to lower our chances of developing liver disease and liver cancer, adds Rebecca West, a specialist liver nurse manager at the charity.
“About nine in 10 cases of liver damage are preventable with lifestyle adjustments,” she adds. So what dangers should we be aware of?
‘MODERATE’ DRINKING
“When alcohol is broken down by the liver, it produces harmful chemicals that can damage and kill liver cells,” says Rebecca. “Although the liver is very good at repairing itself, if it can’t keep up with the damage from regularly drinking too much alcohol, this can cause scarring which builds up and leads to cirrhosis.
“There are a lot of people who mistakenly believe that you have to be alcohol dependent to develop liver disease.
“But if you’re someone who regularly drinks over the NHS recommended limit of around 14 units per week (roughly six pints of beer or six 175ml glasses of 13% ABV wine), you could be increasing your risk of developing liver disease, or liver cancer.”
The British Liver Trust has reported alarming new statistics indicating that more women are suffering from liver disease than ever before. In 2022, more than 2,700 women died from alcohol-related liver conditions, marking the highest number on record. This reflects a 78% increase over the past 20 years and a notable 31% jump since 2019.
What’s more, the age at which women are being diagnosed is getting younger, a trend the Trust is witnessing on their helpline, which is currently receiving an increasing number of calls from women in their forties who have recently been diagnosed.
“We recommend cutting down the amount of alcohol you drink and trying to have at least three days in a row every week without any alcohol at all,” says Rebecca.
OBESITY
“The risks of carrying extra weight, particularly around the abdomen, are already well known, but too many people are still unaware of the damage this could be causing to their liver,” says Rebecca.
“Fatty liver disease, which is also known as MASLD (metabolic dysfunction-associated steatotic liver disease) and NAFLD (non-alcohol related fatty liver disease) is estimated to affect up to one in five people in Britain. It occurs when there is excess fat around the liver, and it can potentially lead to liver damage,” says Rebecca “It’s closely linked with being overweight as well as with conditions like type-2 diabetes and heart and circulatory disease.”
It’s not all bad news though. “Research has shown a well-balanced diet, being physically active and (if needed) losing weight can reduce liver fat and in some cases reverse MASLD,” she adds.
A good goal is to try to lose 10% of your body weight. A BMJ study found this can reduce liver fat, resolve inflammation and reduce fibrosis (scarring).
VIRAL HEPATITIS
“Hepatitis B and C are viruses that can cause serious liver disease if left untreated,” says Rebecca. “They are passed on through blood, for example during childbirth or by sharing items that can get blood on them like razors or needles. Hepatitis B is much more common in other parts of the world, so you are more likely to have it if you or your parents were born overseas.”
Current estimates suggest that less than half of those living with hepatitis B have been diagnosed and more than 60,000 people may be living with chronic hepatitis C without knowing they have it.
One reason for the lack of diagnosis could be that hepatitis often doesn’t exhibit symptoms in the initial stages. There is also a lot of stigma surrounding these viruses, which makes some people reluctant to come forward for testing and treatment.
There are antiviral treatments available for both Hepatitis B and C that can prevent serious liver damage. So if you are concerned, visit your local GP or sexual health clinic to get tested. You can order a free test for Hepatitis C from the NHS (hepctest.nhs.uk).
FOODS THAT ARE ULTRA-PROCESSED
A recent study linked eating too many UPFs with an elevated risk of non-alcoholic fatty liver disease (NAFLD). “A diet high in UPFs, especially the less nutrient-dense kind, is a significant risk factor, as these foods often contribute to increased calorie intake, weight gain, and metabolic dysfunction,” says Nichola Ludlam-Raine, specialist registered dietitian (nicsnutrition.com) and author of How Not To Eat Ultra-Processed (Ebury Press).
“Examples include sugar and artificially-sweetened drinks, ready meals, sugary and processed snacks and other savoury based convenience foods such as crisps.”
Changing eating habits can help – and research suggests that the Mediterranean diet can reduce the risk of NAFLD and improve symptoms of people with the condition. “The Mediterranean diet emphasises whole, minimally processed foods such as vegetables and fruits, whole grains, nuts and seeds, olive oil and oily fish,” says Nichola.
“This diet helps in a few ways. It can reduce inflammation and oxidative stress which can protect liver cells. Also, whole foods that are rich in fibre stabilise blood sugar and prevent insulin resistance, a key driver of NAFLD.
“And replacing saturated fats with mono- and polyunsaturated fats from fish, nuts, and olive oil reduces liver fat.
“The DASH diet (Dietary Approaches to Stop Hypertension) is another liver-friendly approach. It focuses on fruits and vegetables, whole grains, low-fat dairy products and lean protein. Its low-sodium, nutrient-dense profile helps reduce inflammation and improve blood pressure and metabolic markers, which are key in NAFLD prevention and management.
“The aim should be to reduce high fat, sugar, and salt UPFs, while emphasising minimally processed, nutrient-dense foods.”
TOXIC OVERLOAD
“Your liver is responsible for dealing with toxins, including those found in alcohol, cigarette smoke, medicines and household chemicals,” says Rebecca. “It turns these toxins into a non-toxic form that gets passed out of your body when you go to the toilet.”
But having to process too many of these chemicals in one go can end up causing cause overload for our livers. “If your liver gets damaged during this process, it can usually repair itself,” adds Rebecca. “But in rare cases where lots of damage happens suddenly, you can become very ill, so it’s really important to follow instructions and safety advice when taking medicines such as painkillers like ibuprofen, or using household chemicals.”
NOT KNOWING YOUR RISK
“Liver problems develop silently with no obvious symptoms in the early stages, so many people are living their lives completely unaware that they might have liver damage,” says Rebecca. Early signs that your liver might be struggling to function are often attributed to stress or a busy lifestyle.
Things like generally feeling unwell and tired all the time, loss of appetite and disturbed sleep. Other more obvious symptoms, including yellowing of the skin (jaundice), a swollen abdomen and intensely itchy skin can indicate more advanced and serious damage.
Around three quarters of people are currently diagnosed when their liver disease is advanced, and when treatment is less likely to work.
“The liver has a special ability to repair itself, up to a point, so finding out if you have liver damage early gives you a chance to get effective treatment and to change your lifestyle to help stop damage building up over time and leading to serious liver disease,” says Rebecca.
“Because there may not be any symptoms to tell you something’s wrong early on, it’s best to speak to your doctor if you are worried about your liver health,” says Rebecca.
A simple, free online screener test at British Liver Trust (britishlivertrust.org.uk/at-risk-screener) can tell you if you could be at risk of liver disease. The Trust also runs a mobile ‘Love Your Liver’ roadshow that travels the country offering free liver scans. Around one in 10 people scanned at the roadshows have signs of possible liver damage.
■ January is Love Your Liver month. For more advice, visit the British Liver Trust or call their specialist nurse-led helpline on 0800 652 7330
Source link